Ecolab Public Health Experts Discuss Monkeypox and Best Practices to Help Minimise Risk
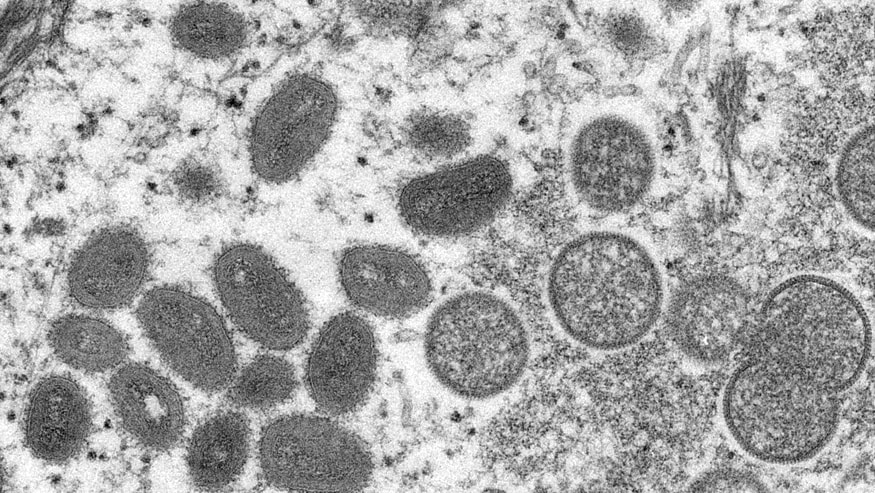
Monkeypox illustration - Photo Credit: CDC- Cynthia S. Goldsmith, Russell Regnery
On July 23, 2022, the World Health Organisation (WHO) declared the global monkeypox outbreak a public health emergency of international concern. Ecolab’s Dr. Elaine Black, director of food safety and public health, and Kaycee Strewler, principal technical account specialist, provide an overview of monkeypox and how to minimise the risks associated with this virus.
- What is monkeypox?
Monkeypox is a rare disease caused by infection with the monkeypox virus, which is part of the same family of viruses as the variola virus, the cause of smallpox. The monkeypox virus is not new – the first human case was recorded in 1970 – however, the current outbreak has spread to many countries where the virus has not been found before.
- What are the signs and symptoms of monkeypox?
A monkeypox infection begins with headache, muscle aches, fever, swollen lymph nodes and exhaustion, followed by the development of a rash or lesions, often initially on the face, then spreading to other parts of the body. Lesions progress through various stages resulting in pustules that scab over and fall off.
The incubation period for monkeypox is usually 7-10 days, but can range 5-21 days, and the illness typically lasts 2-4 weeks. In past outbreaks, monkeypox has caused death in as many as one in every 10 people who become infected, however very few deaths have been reported in the current outbreak. Treatments (antiviral drugs and vaccines) are available and may be region specific and restricted to high-risk populations.
- How does monkeypox transmission occur?
The monkeypox virus spreads between people mostly through direct contact with infectious sores, scabs or body fluids, and can be spread by respiratory secretions, although the extent of respiratory transmission is still under study. The virus also can spread through contact with contaminated surfaces or linens.
While previous outbreaks have been associated with animal-to-human transmission or consumption of meat from an infected animal, the spread of the current outbreak has primarily occurred through prolonged person-to-person contact. At this time, food and water have not been implicated as routes of transmission in the current outbreak.
- What are some best practices to help avoid monkeypox?
Proper hand washing with soap and water is one of the best ways to help avoid the transmission of pathogens. Wash your hands frequently with soap and water or use an alcohol-based hand sanitizer. If your hands are visibly soiled, use soap and water before applying hand sanitizer.
Avoid close, skin-to-skin contact with people who have a rash, and avoid sharing dishes and eating utensils.
Disinfect high-touch hard, non-porous surfaces, including doorknobs, light switches and railings using an EPA-registered disinfectant with an emerging viral pathogen (EVP) claim. Ecolab offers many disinfectants with this claim, including Peroxide Multi Surface Cleaner and Disinfectant (EPA Reg. No. 1677-238) and Disinfectant 1 Wipe (EPA Reg. No. 1677-263). Follow product label directions to ensure proper use.
- What action steps can hotels and other businesses take to help keep employees and customers healthy and help prevent the spread of monkeypox?
There are several steps businesses, particularly those within the hospitality industry, can take to help protect their employees and guests:
- Operators should review and reinforce infection prevention practices with employees (e.g., personal protective equipment (PPE) requirements, hand hygiene practices, proper disinfection of surfaces), and consider facilitating employee education sessions on the signs, symptoms and risk factors for contracting monkeypox.
- Operators should ensure that hand hygiene supplies are readily available at point-of-use in pertinent locations (e.g., restrooms, kitchen or food preparation areas, high-traffic areas such as entrances and exits).
- High-touch hard, non-porous surfaces should be disinfected using an EPA-registered disinfectant with an emerging viral pathogen claim. Eating utensils and dishes should be washed in accordance with the U.S. FDA Food Code.
- Employees should wear appropriate PPE, such as disposable gloves and a well-fitting mask when cleaning or handling linen, particularly in regions known to be high risk for monkeypox or when a person suspected or confirmed to have monkeypox has occupied the area. Ensure soiled linens are contained in a laundry bag or other receptacle and avoid shaking or handling in a manner that may disperse infectious material. Launder linens (e.g., towels, sheets, clothing) following standard laundry protocols including existing Ecolab products and wash formulas.
For more information on monkeypox, click here.
About the Experts:
Dr. Elaine Black, director of food safety and public health for Ecolab, is a public health specialist and microbiologist who leads programme and policy initiatives, including engagement with key customers and professional organizations.
Kaycee Strewler, M.S., principal technical account specialist for Ecolab, is a public health specialist within the company’s Institutional division and serves as a technical consultant for global corporate account customers, providing public health guidance and best practices for personal and environmental hygiene.


